Almost one half of women who have had a baby have some degree of pelvic organ prolapse. Prolapse means “to drop” or “to sink.” Pelvic support problems also can occur in women who have never had children. Most women with these problems have minor symptoms or no symptoms at all. For women with symptoms, proper diagnosis and treatment can bring relief. This page explains:
- pelvic organ prolapse and its symptoms
- causes of pelvic organ prolapse
- types of pelvic support problems
- diagnosis and treatment options
Pelvic Organ Prolapse
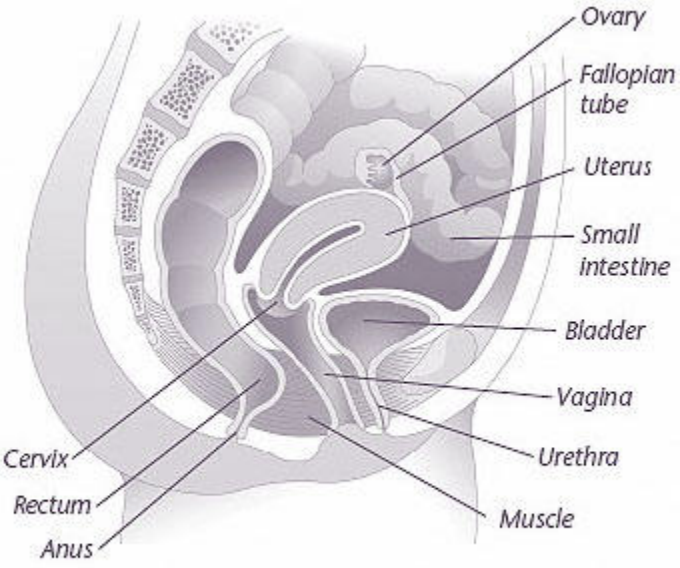
The pelvic organs include the vagina, cervix, uterus, bladder, urethra, and the small intestines and rectum. The pelvic organs are held in place by muscles of the pelvic floor. Layers of connective tissue called fascia also provide support.
Pelvic organ prolapse occurs when the fascia and muscles can no longer support the pelvic organs. These supporting muscles and fascia may become torn or stretched, or they may weaken because of aging. As a result, the organs that they support can drop downward. Sometimes, a bulge can be felt inside the vagina. In severe cases, organs may protrude from the vaginal opening
Symptoms
Many women have no symptoms and are not bothered by their pelvic organ prolapse. A woman may only have felt a bulge of tissue inside her vagina or her health care provider may have noticed it during a physical exam. The symptoms of those who do have problems can range from mild to severe. Listed are common symptoms of pelvic organ prolapse:
- Feeling of pelvic heaviness or fullness
- Bulge in the vagina
- Organs bulging out of the vagina
- Pulling or aching feeling or a feeling of pressure in the lower abdomen or pelvis
- Lower back pain
- Leakage of urine (urinary incontinence) or problems having a bowel movement
- Needing to push organs back up into the vagina to empty the bladder or have a bowel movement
- Sexual difficulties
- Problems with inserting tampons or applicators
- Pelvic pressure that gets worse with standing, lifting, or coughing or as the day goes on
Causes
Pelvic organ prolapse is caused by injury to the muscles or supporting tissue of the pelvic floor. The main cause of this type of injury is having had children. Women who have had a vaginal delivery have a slightly increased risk of pelvic support problems than those who have had a cesarean delivery.
Other causes of pelvic support problems are prior pelvic surgery, menopause, aging, and intense physical activity. Also, factors that add more pressure on the abdomen can cause pelvic organ prolapse, such as being overweight or obese, being constipated and straining to have a bowel movement, and chronic coughing. Heredity is another important factor. This problem runs in families.
Types of Pelvic Support Problems
There are many types of prolapse:
- Uterine prolapse—uterus
- Vaginal vault—top of the vagina
- Cystocele—bladder
- Urethrocele—urethra
- Enterocele—small intestine
- Rectocele—rectum
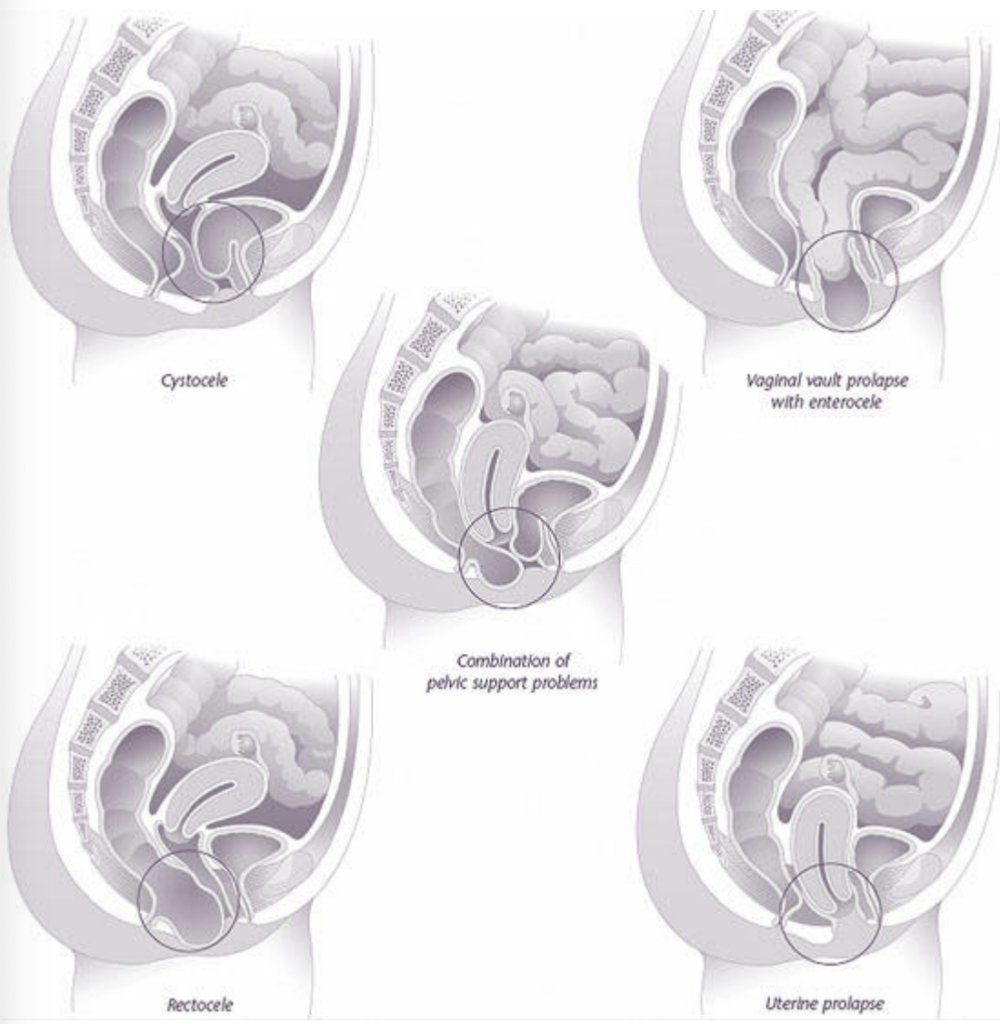
Uterine Prolapse and Vaginal Vault Prolapse
When the uterus drops into the vagina, it is called uterine prolapse. The distance the uterus drops may vary. Mild degrees of prolapse are common. They often do not cause symptoms and do not need surgery.
Women with more severe forms of this condition often will have a feeling of pelvic pressure or a pulling feeling in the vagina or lower back. The cervix may stick out from the vagina. This may cause discomfort or problems with sex.
When the top of the vagina—the “vaginal vault”—loses its support and drops, it is called vaginal vault prolapse. This problem occurs most often in women who have had a hysterectomy. The degree of prolapse varies. Women who have vaginal prolapse may have problems with bladder and bowel function as well as sexual problems.
Cystocele and Urethrocele
A cystocele occurs when the bladder drops from its normal place into the vagina. Urine may leak when there is a sudden increase in abdominal pressure caused by walking, laughing, lifting, or sneezing. The amount of urine lost may be only a few drops or it may be enough to require changing clothes or wearing pads.
In some women, cystoceles may create a kink in the urethra and cause problems with the passing of urine. If this occurs, they may have to strain or push the bladder up by reaching into the vagina to pass urine. A large cystocele may cause the bladder to not empty completely.
Small cystoceles are common. They usually do not cause urination problems and do not need surgery. If you are leaking urine or having symptoms, see your health care provider.
A urethrocele happens when the urethra bulges into the vagina. It often occurs with a cystocele.
Rectocele and Enterocele
When the rectum bulges into or out of the vagina, it is called a rectocele. A large rectocele may make it hard to have a bowel movement, especially if a woman is constipated. Some women must push the bulge into the vagina to have a bowel movement.
An enterocele is a type of support problem that forms when the small intestine pushes against the back wall of the vagina, creating a bulge. Enteroceles often occur with vaginal vault prolapse.
Diagnosis
Proper diagnosis is key to treating pelvic support problems. The exact cause of the problem must be found before the best treatment can be given. Being open about symptoms can be helpful in finding the exact cause.
The health care provider will obtain a medical history and do a thorough exam, including a vaginal and rectal exam. A woman with prolapse may be examined while lying down or while she is standing. She may be asked to strain or cough during the exam to see if she leaks urine. How completely her bladder empties also may be checked.
Treatment
Many women do not need treatment. At regular check-ups the health care provider will keep track of the problem. If symptoms become bothersome, treatment may be needed. Treatment decisions are based on the following factors:
- Age
- Desire for future children
- Sexual activity
- Severity of symptoms
- Degree of prolapse
- Other health problems
No form of treatment is guaranteed to solve the whole problem. Symptoms such as back pain, pelvic pressure, and painful sex may not be relieved by surgery to repair the prolapse. However, the chances of getting some degree of relief are quite good.
Symptom Relief
Changes in diet and lifestyle may be helpful in relieving specific symptoms. If incontinence is a problem, limiting fluid intake, including drinks that contain caffeine (a diuretic), may be helpful. Bladder training (in which you empty your bladder at scheduled times) also may be useful for women with incontinence. Women with bowel problems may find that increasing the amount of fiber in their diets prevents constipation and straining during bowel movements. Sometimes a laxative or medication that softens stools is prescribed. If a woman is overweight or obese, weight loss can help improve her overall health and possibly her prolapse symptoms.
Special Exercises
Exercises called Kegel exercises, or pelvic floor exercises, are used to strengthen the muscles that surround the openings of the urethra, vagina, and rectum (see below “Kegel Exercises”). Doing these exercises regularly may improve incontinence. A health care provider can help a woman be sure she is doing these exercises correctly.
Kegel Exercises
Kegel exercises tone the pelvic muscles. They strengthen the muscles that surround the openings of the urethra, vagina, and rectum. Here is how they are done:
- Squeeze the muscles that you use to stop the flow of urine. This contraction pulls the vagina and rectum up and back.
- Hold for up to 10 seconds, then release.
- Do 50 contractions a day for 4–6 weeks.
Make sure you are not squeezing your stomach, thigh, or buttocks muscles. You also should avoid holding your breath as you do these exercises.
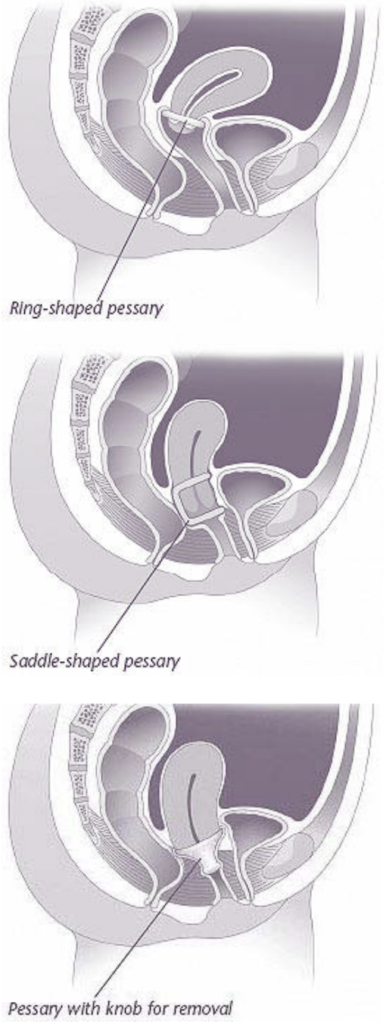
Pessaries
A pessary is a device that is inserted into the vagina to support the pelvic organs. Many women find relief of their symptoms with pessary use.
Pessaries are available in many shapes and sizes. They can be used for short-term or longterm treatment. Pessary choice is based on a woman’s symptoms and the type of prolapse. They can be fitted in most women with prolapse, regardless of type, and some can be used by women who are sexually active.
A health care provider can help find the right pessary that fits comfortably. Some pessaries are designed to be removed, cleaned, and reinserted by the user; for others, a woman must see her health care provider on a regular basis.
Surgery
Some pelvic support problems may be corrected by surgery to restore the normal depth and function of the vagina. The surgery can be done through the vagina or abdomen based on the type of support problem. Surgery may relieve some, but not all, of the symptoms caused by pelvic organ prolapse.
Women who want to have children should consider having them before they have surgery for pelvic support problems. If a woman with a pelvic support problem does become pregnant, she can discuss with her health care provider the best way to give birth and prevent future prolapse.
Many women with prolapse also have problems with urine leakage. Some women begin to have this problem after having surgery to correct prolapse. During surgery, doctors now often include a procedure to prevent or improve incontinence.
Prolapse can recur after surgery. The factors that caused a woman to have prolapse in the first place can cause it to occur again.
Finally…
Many women have some degree of pelvic organ prolapse, although not all women with this problem have symptoms. If you have symptoms that bother you, talk to your health care provider. The right diagnosis and treatment can bring relief.
Glossary
Bladder: A muscular organ in which urine is stored.
Cervix: The lower, narrow end of the uterus, which protrudes into the vagina.
Cesarean Delivery: Delivery of a baby through incisions made in the mother’s abdomen and uterus.
Cystocele: Bulging of the bladder into the vagina.
Diuretic: A drug given to increase the production of urine.
Enterocele: Bulging of the small intestine into the upper part of the vagina.
Fascia: Tissue that supports the organs and muscles of the body.
Hysterectomy: Removal of the uterus.
Incontinence: Inability to control bodily functions such as urination.
Laxative: A product that is used to empty the bowels.
Pelvic Floor: A muscular membrane at the base of the abdomen attached to the pelvis.
Pessary: A device inserted into the vagina to support sagging organs.
Rectocele: Bulging of the rectum into the vaginal wall.
Rectum: The last part of the digestive tract.
Urethra: A tube-like structure through which urine flows from the bladder to the outside of the body.
Urethrocele: Protrusion of the urethra into the vaginal wall.
Uterine Prolapse: Sagging of the uterus into the vagina.
Uterus: A muscular organ located in the female pelvis that contains and nourishes the developing fetus during pregnancy.
Vagina: A tube-like structure surrounded by muscles leading from the uterus to the outside of the body.
Vaginal Vault Prolapse: Bulging of the top of the vagina into the lower vagina or outside the opening of the vagina.
Source: acog.org
