Leakage of urine is called urinary incontinence. It is a common problem in women. Some women occasionally leak small amounts of urine. At other times, leakage of urine is frequent or severe. Often, women with this condition are too embarrassed to tell their health care providers about their symptoms. However, with proper diagnosis, urinary incontinence can most often be treated. This page explains:
- types and symptoms of urinary incontinence
- some of the causes of this condition
- diagnosis and treatment
Types
“Urinary incontinence” is a general term. There are, in fact, different kinds of urinary incontinence. Sometimes, a woman may have more than one of the following types:
- Stress incontinence—In this type, a woman leaks urine when she coughs, laughs, or sneezes. Leaks also can happen when a woman walks, runs, or exercises. It is caused by a weakening of the tissues that support the bladder or the muscles of the urethra. Stress incontinence is the most common type in younger women.
- Urge incontinence—A woman may have a sudden strong urge to urinate and leaks urine before she can get to the bathroom. This type sometimes is called overactive bladder. It occurs if the muscles of the bladder are too active and contract too often. It also can be caused by problems with the nerves that send signals to the bladder.
- Mixed incontinence—A woman has symptoms of both stress and urge incontinence. This combination may cause more urine to leak than either type alone would.
- Overflow incontinence—A woman has steady leaks of small amounts of urine. This type occurs when the bladder does not empty all the way during voiding. The bladder muscle may not be active enough, or the urethra may be blocked.
Symptoms
In addition to leaking urine, a woman with incontinence also may have other symptoms:
- Urgency—A strong urge to urinate whether or not the bladder is full, often with pelvic pressure
- Frequency—Voiding more often than a woman considers usual
- Nocturia—The need to void during hours of sleep
- Dysuria—Painful urination
- Enuresis—Bed-wetting or leaking urine while sleeping
Incontinence does not always mean that a woman leaks large amounts of urine, or leaks often. For some women, leaking even a small amount, or having symptoms once a week or even less often, is a problem. Others do not consider urine leakage to be a problem and simply make changes in lifestyle, such as
wearing absorbent pads. If you have symptoms of urinary incontinence, tell your health care provider. If the symptoms bother you, and they are having a negative effect on your life, you may want to seek treatment.
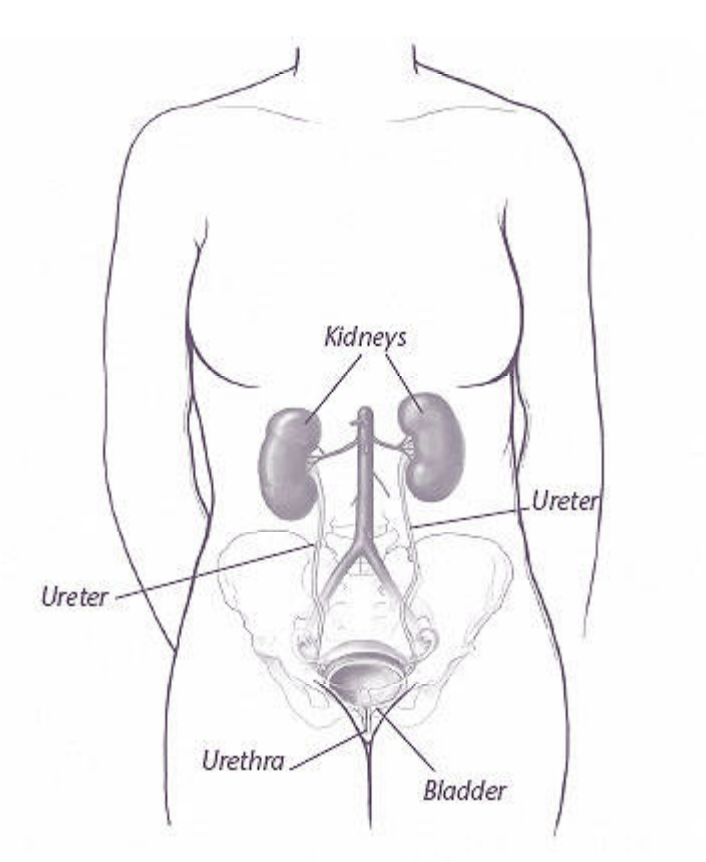
The Female Urinary Tract
The urinary tract is made up of the kidneys, ureters, bladder, and urethra. During urination (also called voiding), the muscles around the urethra relax. The muscle that lines the bladder then contracts, and urine flows to the urethra and out of the body. When the bladder is almost empty, the muscles around the urethra contact. The bladder muscle relaxes, and the urine stops flowing.
Causes
There are many causes of urinary incontinence. Some are short-term and easier to treat than others. Sometimes, more than one cause is responsible for a woman’s urinary incontinence.
Short-term Causes
- Urinary tract infection—Loss of bladder control may be caused by an infection of the urinary tract. Infections of the bladder (cystitis) are common in women. Signs of an infection include pain, frequent urination, and sometimes blood in the urine. Urinary tract infections are treated with antibiotics. Loss of urine may stop when the infection is cured.
- Medications—Loss of bladder control may be a side effect of some medications, such as diuretics or other blood pressure medications. If a medication is causing this side effect, the medication sometimes can be changed or the dosage adjusted by your health care provider.
- Abnormal growths—Polyps, bladder stones, or less commonly, bladder cancer, can cause urinary incontinence. Abnormal growths often cause urge incontinence and may be associated with blood in the urine. If you see blood in your urine, or if you are unsure about the source of any bleeding, it is important to alert your health care provider right away.
Long-term Causes
- Pelvic support problems—The pelvic organs are held in place by supportive tissues and muscles. Weakening or stretching of these supports may be caused by pregnancy, childbirth, or aging. As a result of this weakening, the organs that they support may sag out of place. If the tissues that support the urethra, bladder, uterus, or rectum become weak, these organs may drop down, causing urine leakage or making it hard to pass urine.
- Urinary tract abnormalities—A fistula is an abnormal opening from the urinary tract into another part of the body, such as the vagina. It can allow urine to leak out through the vagina. A fistula may result from pelvic surgery, radiation treatment, advanced cancer of the pelvis, or, in rare cases, a difficult delivery.
- Neuromuscular problems—In some neuromuscular problems (disorders that affect muscle control), the signals from the brain and spinal cord do not connect properly with the bladder and urethra. The result can be leakage of urine. Neuromuscular problems often occur in conditions such as diabetes mellitus, stroke, or multiple sclerosis.
Diagnosis
A number of steps may be needed to find the cause of urinary incontinence. Knowing the cause helps your health care provider suggest the best treatment for you.
Your health care provider will ask you about your past medical history. You also will be asked about factors that may affect your urination habits. A voiding diary or daily log of urination is a useful tool your health care provider may suggest. You may be asked to record the time and amount of urine leakage, often for 3 days. You also should note how much liquid you drank and what you were doing when a leak occurred.
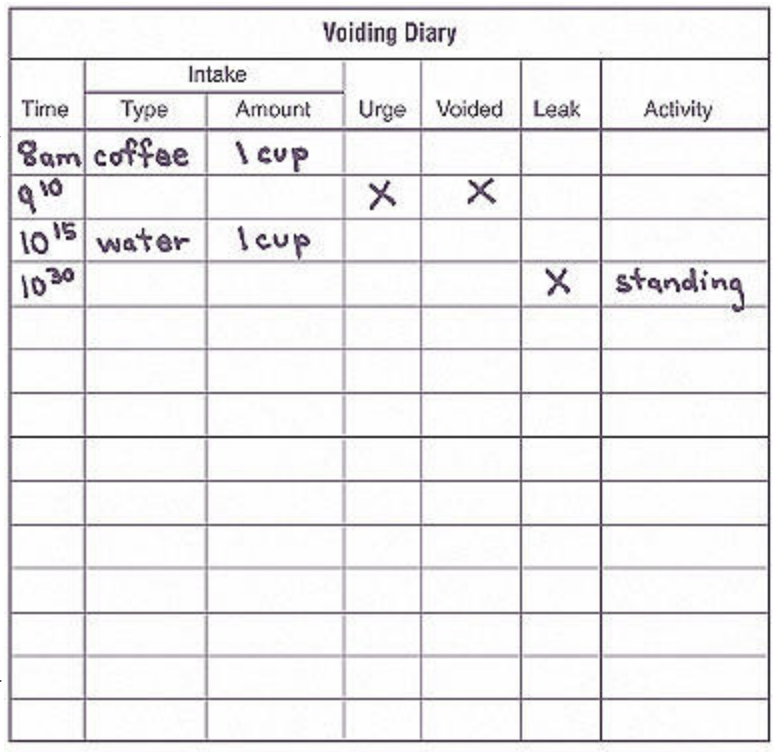
Your health care provider may ask you to keep a voiding diary to record the time and amount of urine leakage.
A pelvic exam will be done to detect physical conditions that might be causing the incontinence, such as a pelvic support problem. Lab tests also may be done to look for signs of a urinary tract infection. The following tests also may be performed:
- Urodynamic tests— The bladder is filled through a catheter, a narrow tube that is inserted into the urethra, and the function of the bladder and urethra are checked. You may be asked to push down, cough, or urinate as part of this test.
- Postvoid residual volume test—The amount of urine that is left in the bladder after urinating is measured with an ultrasound device or by placing a catheter in the bladder.
- Stress test—During a stress test, you are asked to cough a few times with a full bladder. Any loss of urine is recorded.
- Cystoscopy— A thin, lighted tube with a camera lens at the end is used to look inside the bladder and urethra.
- Dye test—A pad is worn after a nontoxic dye is put in the bladder. If the pad gets stained with the dye, there was a loss of urine.
Treatment
Options for treating incontinence include lifestyle changes, bladder training, physical therapy, the use of devices that are placed in the vagina, medications, bulking injections, and surgery. Your health care provider may first suggest nonsurgical treatment. Often, several treatments are used together for the best effect. If other treatments do not improve the problem, surgery may help.
Lifestyle Changes
Making the following changes in your lifestyle, if they apply to you, may help decrease the number of times you leak urine:
- Lose weight. In overweight women, losing weight has been shown to decrease the frequency of urine leakage.
- Avoid constipation. Repeated straining from trying to empty the bowels may damage the pelvic floor.
- Drink less fluids and limit intake of caffeine. Many women have heard the advice to drink eight glasses of water a day. This amount, however, does not take into account individual factors such as age, body weight, activity, and the outside temperature. If you have incontinence, it may be a good idea to monitor how much you drink. A good way to tell whether you are drinking the right amount of fluids is to check your urine and adjust your fluid intake accordingly. If it is dark and has a strong smell, you are not drinking enough. If it is pale or has no color, you are drinking too much. Also, be aware that caffeine can act as a diuretic. Caffeine is found in coffee, tea, some soda, and even some over-the-counter medications.
- Seek treatment for frequent coughing. If you have a chronic (long-lasting) cough, and it causes you to leak urine, find out the cause of your frequent coughing. A chronic cough may be a sign of allergies, a sinus infection, or other condition that can be treated.
- Stop smoking. Urinary incontinence is more common and more severe in smokers. The cause of this link is still being studied.
Kegel Exercises
Kegel exercises tone your pelvic muscles. They strengthen the muscles around the openings of the urethra, vagina, and rectum. Just like doing situps, these exercises work only if you use the right muscles, hold the “squeeze” long enough, and do enough of them.
- Squeeze the muscles that you use to stop the flow of urine.
- Hold for up to 10 seconds, then release.
- Repeat 10–20 times at least 3 times a day.
Be careful not to squeeze the muscles of the leg, buttock, or abdomen. Do these exercises on a regular basis. It may take 4–6 weeks to notice an improvement in urinary incontinence symptoms.
Bladder Training
Bladder training has been shown to be helpful in treating urge urinary incontinence. The goal of bladder training is to learn how to control the urge to empty the bladder and increase the times between urinating to normal intervals (every 3–4 hours during the day and every 4–8 hours at night). After a few weeks of this training, you may leak urine less often.
Physical Therapy
Kegel exercises can help strengthen the pelvic muscles (see “Kegel Exercises”). These exercises are helpful in all types of incontinence. Kegel exercises, along with bladder training and modifying fluid intake, are often very successful in treating stress and urge incontinence.
If you have trouble doing Kegel exercises, you may want to see a physical therapist who specializes in women’s pelvic health. Biofeedback is a training technique that may be useful if you have problems locating the correct muscles. In biofeedback, sensors are placed inside or outside the vagina. These sensors measure the force of pelvic muscle contraction. When you contract the right muscles, you will see the measurement on a monitor. This feedback lets you know that you are doing Kegel exercises in the right way.
If your muscles are too weak and you cannot perform a Kegel contraction at all, other therapies, such as electrostimulation, can be done. In electrostimulation, the pelvic muscles are made to contract with special electrodes. These contractions strengthen the muscles so that Kegel exercises become possible.
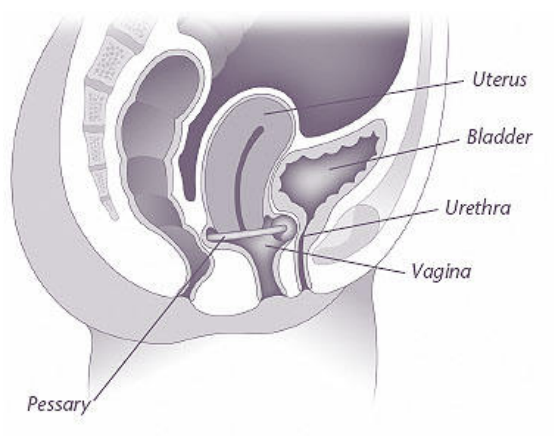
Using a Pessary
A pessary is a device that is placed into the vagina. It supports the pelvic organs and may help prevent urine leakage.
Devices
A pessary is a device that is inserted into the vagina to treat pelvic support problems and urinary incontinence. Pessaries support the pelvic structures, and some compress the urethra. Pessaries come in all shapes and sizes. Most support pessaries are shaped like rings or dishes. There also are specially designed pessaries for urinary incontinence. They are useful for women who do not want or cannot have surgery to correct their incontinence.
Support pessaries generally can be removed and inserted by the patient. Pessaries cannot be used by everyone. However, for many women, pessaries provide relief of symptoms without surgery.
Medications
Drugs that help control muscle spasms or unwanted bladder contractions can help prevent leaks associated with urge incontinence. These medications also can help reduce the frequency of urination. Your health care provider will help you decide which drug is most likely to work best for you. Side effects of some of these drugs include the following:
- Dry mouth
- Constipation
- Nausea
- Blurred vision
- Change in sleeping patterns
Bulking Agents
These agents may be used when the sphincter muscle of the urethra is very weak and extensive surgery is not an option or has not worked. A substance is injected into the tissues around the urethra to add bulk. The urethra becomes narrowed, decreasing leakage. This procedure can be done in a doctor’s office or clinic.
Surgery
Surgery can be done to treat stress urinary incontinence. You and your health care provider may discuss many factors before choosing the surgery that is right for you:
- Age
- Lifestyle
- Need for hysterectomy or treatment of other pelvic problems
- Medical history (if you have had radiation therapy for pelvic cancer or have already had surgery for incontinence)
- General health
- Cause of the problem
Surgical techniques to correct urinary incontinence involve the following approaches:
- Slings—Different materials are currently being used as slings to lift or provide support for the urethra. Each type of sling has advantages and disadvantages. You should discuss each type with your health care provider if you are interested in this kind of surgery.
- Colposuspension—Stitches are suspended across the neck of the bladder and the first part of the urethra and attached to tissue on either side. These stitches lift up the bladder and urethra and hold them in place.
Finally…
Loss of bladder control is a common problem and there are many treatment options available. If you have symptoms that affect your daily life, tell your health care provider. A complete and thorough exam is needed to find the cause of the problem. Most cases of urinary incontinence can be greatly improved with treatment.
Glossary
Antibiotics: Drugs that treat infections.
Biofeedback: A technique in which an attempt is made to control body functions, such as heartbeat or blood pressure.
Bladder: A muscular organ in which urine is stored.
Catheter: A tube used to drain fluid or urine from the body.
Cystitis: An infection of the bladder.
Cystoscopy: A test in which the inside of the urethra and bladder are examined.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Diuretics: Drugs given to increase the production of urine.
Dysuria: Pain during urination.
Fistula: An abnormal opening or passage between two internal organs.
Hysterectomy: Removal of the uterus.
Nocturia: The need to urinate frequently during the night.
Pelvic Exam: A manual examination of a woman’s reproductive organs.
Pessary: A device inserted into the vagina to support sagging organs.
Polyps: Benign (noncancerous) growths that develop from tissue lining an organ, such as that lining the inside of the uterus.
Stroke: A sudden interruption of blood flow to all or part of the brain, caused by blockage or bursting of a blood vessel in the brain and often resulting in loss of consciousness and temporary or permanent paralysis.
Ultrasound: A test in which sound waves are used to examine internal structures.
Urethra: A tube-like structure through which urine flows from the bladder to the outside of the body.
Uterus: A muscular organ located in the female pelvis that contains and nourishes the developing fetus during pregnancy.
Vagina: A tube-like structure surrounded by muscles leading from the uterus to the outside of the body.
Voiding Diary: A daily log in which a woman keeps track of how many times she urinates, her fluid intake, and the number of times she leaks urine.
Source: acog.org
