Endometrial polyps are one of the most common causes of abnormal vaginal bleeding in both premenopausal and postmenopausal women. The likelihood of developing endometrial polyps appears to increase with age. Risk factors for developing endometrial polyps include Tamoxifen (used to treat breast cancer), hormone replacement therapy, hypertension and obesity.
Endometrial polyps are occasionally found in women who are not experiencing any symptoms at all. They may show up on a pelvic ultrasound examination or even as an incidental finding on a CT scan of the pelvis done for entirely different issues such as hip pain.
The precise diagnosis of an endometrial polyp can only be made by removing it and having it examined by a pathologist. Occasionally a polyp resembles a uterine fibroid — they can easily be confused with one another on ultrasound and hysteroscopy.
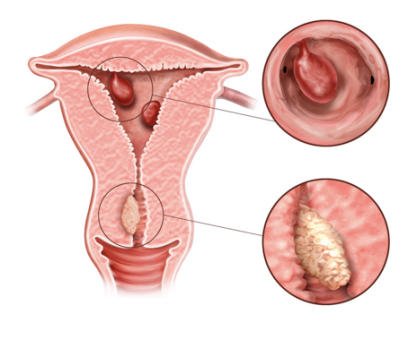
What are endometrial polyps?
The uterus contains two types of tissue—endometrium (lining tissue) and myometrium (muscle tissue). The endometrium covers the inside of the uterus. Both endometrium and myometrium can form benign and malignant tumors—fortunately, in both cases the benign ones are much more common.
When the endometrium forms an overgrowth (tumor) of cells it forms a finger-like projection called an endometrial polyp. While these polyps are generally benign they occasionally contain either malignant or premalignant cells – this is called endometrial hyperplasia.
Because of the potential for polyps to contain malignant or pre-malignant cells they should be removed and sent for analysis.
How often are endometrial polyps malignant?
The risk of malignant is greater in postmenopausal women than premenopausal women. In postmenopausal women the risk of malignancy is approximately 5.4% while it is approximately 1.7% in premenopausal women.
If a polyp is suspected on ultrasound what is done to establish the diagnosis?
To be certain of the existence of an endometrial polyp we recommend a diagnostic hysteroscopy and removal (polypectomy). These two procedures are often easy to combine into a single procedure.
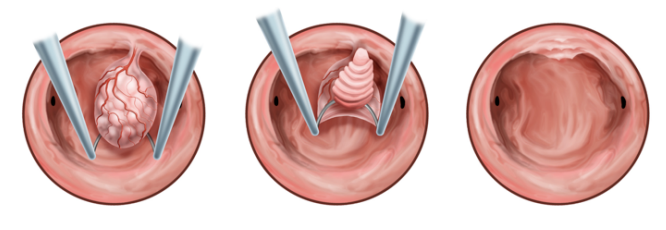
How do you remove polyps?
Polyps and fibroids are removed the same way. The procedure we perform in office to remove these polyps is the Myosure procedure. We insert an instrument into the uterus called an operative hysteroscope—also called a resectoscope. The instrument is attached to a small camera that allows the image to be projected onto a monitor. In this way we can also introduce an electrode that allows us to remove the polyp by cutting it at its attachment point. The procedure generally takes from 5-10 minutes to perform and is called a hysteroscopic (or resectoscopic) polypectomy.
What can I expect aftwards?
You will likely be observed for an hour following the procedure but should plan on spending 2 hours here from the moment you arrive. You’ll wish to rest most of the day after the procedure. If you’ve having a simple polypectomy with no other procedure you will experience some bright red bleeding for about 4-5 days. This will be followed by a brown discharge for another week until it stops entirely. You may be asked to take 24 to 48 hours off from work depending on your own individual circumstances.
Can endometrial polyps come back?
The short answer is yes. In about 10-15% of cases they recur. For this reason we occasionally suggest removal of the entire lining—which is where polyps originate from. This is only offered under very specific circumstances. For women who still wish to retain their ability to have children this is never offered as an option.
References: Lee SC, Kaunitz AM, Sanchez-Ramos et al. The oncogenic potential of endometrial polyps: a systematic review and meta-analysis. Obstet Gynecol. 2010; 116:1197; Paradisi R, Rossi S, Scifo MC, et al. Recurrence of endometrial polyps. Gynecol Obstet Invest. 2014; 78:26-32.
