Midlife often is called “the prime of life,” and research suggests it really is. At midlife, you are likely to be healthy and productive. By this stage, you’ve likely met goals set in your youth and are thinking about where to go next in your life. However, myths about middle age abound. Some people think of it as a dreary stage when the best that life has to offer is over. Nothing is further from the truth.
What is true is that midlife is a busy time, full of changes. Maybe your children are older—even living on their own—giving you free time you haven’t had in years. You may switch to a new career, go back to school, or take up new hobbies.
Your body changes at midlife, too. Around your mid-40s, you enter a transition phase called perimenopause. It is a time of gradual change leading up to and following menopause. In general, perimenopause extends from age 45 years to age 55 years, although the timing varies among women. During this time, the ovaries produce less estrogen. Other changes occur in your body, as well. Because these changes happen slowly over time, you may not be aware of them.
Menopause is sometimes called “the change of life.” It marks the end of menstrual periods and of your childbearing years. On average, the age at which American women have their last menstrual period is 51 years.
Perimenopause and menopause are natural events. Although the same basic changes take place inside all women’s bodies, each woman feels and copes differently. The symptoms of menopause may first arise in perimenopause as early signals. No two women seem to experience menopause in exactly the same way. It’s best to approach menopause fully informed and with a positive mind-set. By knowing what to expect, you can take steps to ease symptoms and prevent health problems later in life.
Both women and men face midlife changes and must deal with them. These changes in women may be more pronounced as hormone levels decrease more dramatically than in men. Sharing this page with your partner may help promote communication during this time.
Your Menstrual Cycle
During your childbearing years, monthly changes in two hormones—estrogen and progesterone—bring about menstrual bleeding. Your ovaries make these hormones. The ovaries also make other hormones, including the male hormone testosterone.
The ovaries contain thousands of eggs. Each month, an egg matures and is released by one ovary. This is called ovulation. Only about 400 eggs are released over a woman’s lifetime. The rest are absorbed into the body.
Estrogen and progesterone prepare your body for pregnancy. Estrogen is produced throughout the menstrual cycle. Progesterone is produced only during the second half of the cycle. These hormones cause the endometrium (lining of the uterus) to grow and thicken each month. The endometrium nourishes an egg that has been fertilized by a man’s sperm. If the egg is not fertilized, hormone levels decrease. This signals the uterus to shed its lining. This shedding is your monthly period.
As a woman approaches menopause, there is not enough estrogen to thicken the uterine lining, and menstrual periods stop. Ovulation also stops. A woman can be sure she has entered menopause when she has not had a menstrual period for 1 year. However, a woman is not completely without estrogen after menopause. It continues to be made by other glands and by body fat, but generally there is less of it than before menopause.
Symptoms and Effects
Some women compare perimenopause to puberty—another time when you have to adjust to big changes. These changes may make you feel unlike your usual self. Many changes of perimenopause are related to a decrease in estrogen levels. Some are related to aging. The effects caused by the lack of estrogen can be treated. Hormone therapy (HT) can relieve symptoms as well as protect against certain diseases, such as osteoporosis.
Menstruation
In your 40s, increasing and decreasing hormone levels can cause changes in your menstrual cycle. These changes can be erratic. For instance, the number of days between periods may increase or decrease. Your periods may become shorter or longer. Flow may get heavier or lighter. You may begin to skip periods. Some months your ovaries may release an egg, some months they may not.
Although changes in bleeding are normal as you near menopause, they still should be reported to your doctor. Abnormal bleeding can sometimes be a sign of other problems. Your doctor can assess your symptoms. See your doctor if you:
- Notice a change in your monthly cycle
- Have very heavy bleeding
- Have bleeding that lasts longer than normal
- Bleed more often than every 3 weeks
- Bleed after sex or between periods
Hot Flushes
As you approach menopause, you may start having hot flushes (also known as hot flashes). About 75– 85% of perimenopausal women get them. These flushes are the most common symptom of perimenopause.
A hot flush is a sudden feeling of heat that rushes to the upper body and face. The skin may redden like a blush. You may break out in a sweat. A hot flush may last from a few seconds to several minutes or longer.
Hot flushes may come a few times a month or several times a day, depending on the woman. Some women will get hot flushes for a few months, some for a few years, and some not at all.
Hot flushes can happen anytime— day or night. Those occurring during sleep, called night sweats, may wake you up and leave you tired and sluggish the next day. Even though hot flushes are a nuisance, are sometimes embarrassing, and may interfere with daily life, they are not harmful.
What You Can Do To Handle Hot Flushes
If you have hot flushes, you can take steps to improve your comfort:
- Try to pinpoint what triggers the hot flush and avoid it if you can. You may find that hot drinks like tea or coffee, spicy foods, or alcoholic drinks seem to bring on some of your hot flushes. They also may be set off by stress, hot weather, or a warm room.
- Dress in layers. You can remove pieces of clothing at the first sign of a flush to feel cooler.
- Keep your office or home thermostat low. Have a fan handy—some hand-held types are small enough for your purse.
- Exercise regularly. Some research suggests that women who exercise have fewer and less intense hot flushes.
- See your doctor. You may benefit from hormones or other therapies he or she can prescribe.
Sleep Problems
Perimenopausal women may have to deal with sleep problems. Night sweats may disrupt your rest. You may have insomnia (trouble falling asleep), or you may be awake long before your usual time.
Perimenopausal women may not get enough REM (rapid eye movement) sleep. REM sleep is when dreams occur. A key role of REM sleep is to rest the brain. Without REM sleep, you will not feel rested. When normal sleep rhythms are broken, a woman’s moods, health, and ability to cope may be affected. She may have trouble concentrating or become depressed.
If you are having trouble falling or staying asleep at night, try the following suggestions:
- Stay on a schedule. Go to bed and wake up at the same time every day, including weekends.
- Eat regular meals at regular times. Avoid late meals and filling snacks.
- Avoid caffeine found in coffee, tea, chocolate, and cola drinks. Because caffeine stays in the bloodstream for up to 6 hours, consume as little as possible, and limit it to the morning or early afternoon.
- Avoid nightcaps. Alcohol may make you feel drowsy, but it also affects the pattern of REM and non-REM sleep and may cause you to wake up often during the night.
- Exercise regularly. In general, people who are fit tend to sleep better.
Vaginal and Urinary Changes
As your estrogen levels decrease, changes take place in the vagina. Over time, the vaginal lining gets thin, dryer, and less flexible. Some women have vaginal burning and itching. The vagina also takes longer to become moist during sex. This may cause pain during sex. Vaginal infections also may occur more often. Ways to manage vaginal changes are discussed in the section “Sexuality.”
The decrease in estrogen may thin the lining of the urinary tract and weaken supporting tissues. This can cause women to urinate more often. Also, the bladder may become more prone to infection. When the tissues get weak, some women may leak urine when they sneeze, cough, or laugh. This is known as stress incontinence. Some women get this problem even before perimenopause because their tissues have been stretched by childbirth. If you notice a loss of bladder control, tell your doctor. It often can be treated.
Bones
Once made, bone is always changing. Old bone is removed in a process called resorption, and new bone is formed in a process called formation. From childhood until age 30 years, bone is formed faster than it is broken down. The bones become larger and denser. After age 30 years, the process begins to reverse: bone is broken down faster than it is made. This process continues for the rest of your life. A small amount of bone loss after age 35 years is normal in all women and men. It usually does not cause any problems. However, bone loss that happens too fast can result in osteoporosis. Osteoporosis causes bones to become too thin and weak, which can result in a break and disability.
Are You at Risk?
Certain factors increase your risk of bone fractures:
- Menopause—Bone loss increases after menopause because the ovaries stop making estrogen, which protects against bone loss.
- Removal of ovaries—If a woman has her ovaries removed before menopause, the sudden decrease in estrogen can result in rapid bone loss unless she takes treatment, such as estrogen.
- Personal or family history of fracture
- Diet low in calcium (lifelong)
- Recent falls
- Lack of exercise
- Low body weight (less than 127 pounds)
- Poor health
- Dementia
- Some medications
- Alcohol and tobacco use
- Certain medical conditions
- Use of certain corticosteroids
- Vision problems
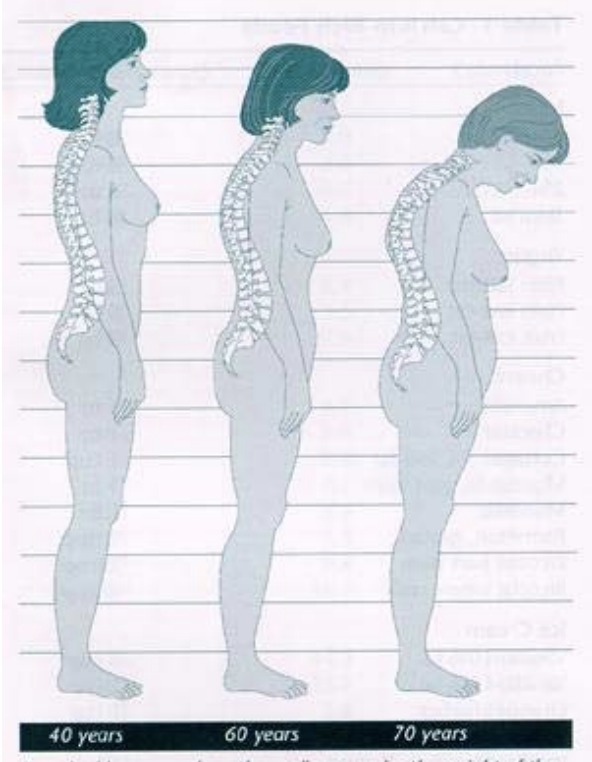
Some later signs of osteoporosis are back pain or tenderness, slight curving of the upper back, and loss of height. When spinal bones weaken and collapse under the weight of the upper body, they can cause a pronounced curve called a dowager’s hump.
Hormone therapy can slow or stop bone loss. For women who cannot take estrogen, there are other medications that may help. Calcitonin is one that slows bone loss. A group of medicines called bisphosphonates has been shown to increase bone density and reduce fractures.
To prevent osteoporosis, you should focus on building and keeping as much bone as you can before menopause. You can do that by getting plenty of calcium and exercise.
Before menopause, you need about 1,000 mg of calcium per day. After menopause, you need 1,500 mg per day. (Women on hormone therapy need only 1,000 mg per day until age 65 years, after which they need 1,500 mg per day.) Milk fortified with vitamin D is a good source. Other good sources of calcium are listed in Table 1. Vitamin D helps the body absorb calcium. Your body makes vitamin D on its own if you get just 15 minutes of sunlight each day. You also can take vitamin D pills, but consult your doctor first. A woman should take the recommended daily amount of vitamin D, which is 400–800 IU (international units).
Just as muscles get stronger with regular exercise, so do bones. Active women have higher bone density than women who do not exercise. Regular weight-bearing exercise is best to strengthen bones and slow bone loss. Brisk walking is good. So are aerobic dancing, stair stepping, tennis, and running. Lifting weights also improves bone strength.
| Food | Amount | Calcium (milligrams) | Fat (grams) | Calories |
| Milk | ||||
| Whole | 8 oz | 288 | 8.0 | 150 |
| 1% | 8 oz | 300 | 2.6 | 102 |
| 2% | 8 oz | 297 | 4.7 | 121 |
| Skim | 8 oz | 302 | 0.4 | 86 |
| Yogurt | ||||
| Plain fat-free | 8 oz | 452 | 0.4 | 127 |
| Plain low-fat | 8 oz | 415 | 3.5 | 144 |
| Fruit low-fat | 8 oz | 314 | 2.6 | 225 |
| Cheese | ||||
| American | 1 oz | 124 | 8.9 | 106 |
| Cheddar | 1 oz | 204 | 9.4 | 114 |
| Cottage, 1% low-fat | 1 cup | 138 | 2.3 | 164 |
| Mozzarella, part skim | 1 oz | 147 | 6.1 | 80 |
| Muenster | 1 oz | 203 | 8.5 | 104 |
| Parmesan, grated | 1 tbsp | 69 | 1.5 | 23 |
| Ricotta, part skim | 1/2 cup | 337 | 9.8 | 171 |
| Ricotta, whole milk | 1/2 cup | 257 | 16.1 | 216 |
| Ice Cream | ||||
| Vanilla, 10% fat | 1 cup | 176 | 14.3 | 269 |
| Vanilla, 16% fat | 1 cup | 151 | 23.7 | 349 |
| Orange Sherbet | 1 cup | 103 | 3.8 | 270 |
| Vanilla Ice Milk, hard | 1 cup | 176 | 5.6 | 184 |
| Vanilla Ice Milk, soft serve | 1 cup | 274 | 4.6 | 223 |
| Seafood | ||||
| Oysters, raw | 12 | 76 | 4.2 | 116 |
| Sardines with bones, canned in oil, drained | 4 | 184 | 5.6 | 100 |
| Pink salmon with bones, canned | 3 oz | 181 | 5.1 | 118 |
| Shrimp, canned, drained | 3 oz | 50 | 1.7 | 102 |
| Vegetables | ||||
| Bok Choy (Chinese Cabbage), raw | 1 cup | 74 | 0 | 9 |
| Broccoli, fresh, cooked | 1 cup | 178 | 0.4 | 46 |
| Broccoli, frozen, cooked | 1 cup | 94 | 0.2 | 50 |
| Soybeans, mature, boiled | 1 cup | 175 | 15.4 | 298 |
| Collards, fresh, cooked | 1 cup | 148 | 0.3 | 27 |
| Turnip Greens, fresh, cooked (leaves and stems) | 1 cup | 198 | 0.4 | 30 |
| Other Foods | ||||
| Tofu | 1 cup | 260 | 11.8 | 366 |
| Orange | 1 | 56 | 0.1 | 65 |
| Almonds | 1 oz | 80 | 14.7 | 167 |
| Calcium-enriched orange juice | 8 oz | 300 | 0 | 120 |
| Calcium-fortified cereal | 1 cup | 600 | 1 | 110 |
Cardiovascular Disease
Heart disease kills more women than any other cause of death. After menopause, a woman’s risk of heart disease and stroke increases. Women who have not reached menopause have a far lower risk of cardiovascular disease than men. The estrogen produced by women’s ovaries before menopause protects them from heart attacks and stroke. When less estrogen is made after menopause, women lose much of this protection. The risk of heart attack and stroke then increases.
Factors other than lack of estrogen can add to your heart disease risk. These include high cholesterol, high blood pressure, smoking, a high-fat diet, diabetes, and obesity. Heart disease is almost twice as likely to strike inactive people than people who exercise regularly. The best exercises to strengthen your heart and lungs are brisk walking, running, swimming, and other aerobic activities. It’s wise to lead a healthy lifestyle overall—including eating healthy foods and not smoking—to ward off heart problems.
Sexuality
Sexuality is an important part of life. Sex can give you a feeling of well-being and bring you closer to your partner. You can continue to enjoy an active sex life well after menopause.
Sexual Changes in Women
Your sex drive and sexual response may change in the perimenopausal years or beyond. As you age, sexual arousal takes longer. It’s important to talk with your partner about what you’re feeling and what excites you. You may need to spend more time on foreplay or try new positions.
When estrogen levels are low, vaginal tissue gets thinner and dryer. This may cause discomfort during intercourse. Water-soluble lubricants sold over-the-counter can help moisten the vagina. Having regular sex may help, too. An active sex life increases blood flow to the genitals and may help you avoid some vaginal changes as you age.
Some postmenopausal women enjoy sex less than they used to because they feel self-conscious about wrinkles and other signs of aging. However, many women say their sex lives are better after menopause. The worry of pregnancy is gone, and they feel more confident and adventurous. A couple may have more time to focus on each other. A wide array of sexual “how-to” books, videos, and devices are available to try together. If you keep an open mind, you may find that sex has more passion than ever.
Sexual Changes in Men
Men take longer to get aroused as they age, just as women do. Their erections may become less rigid, as well. This is normal and should not affect sexual satisfaction.
Some men, however, cannot keep an erection long enough for intercourse. This is called impotence. Almost all men have trouble with impotence at some time in their lives. Impotence may be brought on by certain diseases such as diabetes. Certain drugs and surgeries also can cause it. Impotence also can be related to stress, fear, depression, or emotional problems. If you and your partner are struggling with impotence or other sexual problems, see a doctor. Many solutions are possible.
Emotional Concerns
The constant change of hormone levels during perimenopause can effect a woman’s emotions. Some women have mood swings, memory lapses, and poor concentration. Some may feel irritable or are depressed. These problems do not affect every woman. However, for those affected, it may be hard to cope because they may still be having monthly periods and may think menopause is far in the future.
Lifestyle Changes
Losses, new demands, and changes in routines are common at midlife. Your children may be entering their teen years—a time of challenges. After more than a decade of closeness, your kids may pull away, talk with you less openly, or act in a way that is moody or hostile. These changes are unsettling, to say the least. If your children are grown and out of the house, you may feel less needed.
Today, many women wait to start a family until they are around 40 years of age. Becoming a new mother at midlife—no matter how joyful an event—is a big adjustment. You may find yourself juggling a job, child care, household chores, and feedings at 3 am. If you are a single mother, the challenges are even greater.
On top of it all, you may be caring for young children and aging parents at the same time. Your roles may reverse, and you find yourself “parenting your parents.”
Women who have not had children or never married also face changes of midlife. They may be concerned about their future and lack support in confronting challenges.
Despite these challenges, midlife often is still a rewarding phase of life. You are better equipped emotionally to handle problems than at any other time. You have wisdom and know how to manage things. You may find that turning points have benefits, such as revealing strengths you never knew you had.
How to Cope
The best thing you can do to get through midlife’s rough spots is reach out for help. Talking with others is reassuring. If you open up to a friend, you may find she is facing the same fears and stresses. Counseling and support groups exist for everything from grief and divorce to career changes.
If you are bothered by unsteady emotions or mental lapses, talk to your doctor. Most likely you are not “going crazy,” as many women fear, but instead are dealing with perimenopausal symptoms. There are therapies that can help. Sometimes, just knowing what is wrong can bring relief.
Hormone Therapy
A major decision facing you as you enter menopause is whether to take HT. For many women it is a confusing issue. It’s important to learn as much as you can about HT and discuss options with your doctor, in light of your health and family history.
What Is Hormone Therapy?
With HT, you are given estrogen to replace the estrogen your body is no longer making. If you have never had a hysterectomy and, therefore, still have a uterus, you normally are given progestin, as well. This helps reduce the risk of cancer of the lining of the uterus that occurs when estrogen is used alone. The progestin may be taken every day with estrogen, or estrogen may be taken on some days and progestin added on others.
Estrogen often is prescribed as a pill you take daily or a patch you wear on your skin. Estrogen also is available as a vaginal ring. This ring is placed inside the vagina and releases small doses of estrogen to relieve dryness and urinary tract problems. There also are vaginal creams that are prescribed to relieve specific symptoms, such as vaginal dryness. When progestin is prescribed, it usually is given as a pill.
Oral contraceptives (birth control pills) also contain estrogen and progestin, but in higher doses. During perimenopause, oral contraceptives offer birth control and help regulate the menstrual cycle. They may be used during perimenopause before HT. Oral contraceptives may not be used in women who smoke because there is a risk of blood clots with higher doses of oral contraceptives.
Benefits of Hormone Therapy
One benefit of HT that women are likely to notice right away is the relief from symptoms. For about 98% of women who take estrogen, hot flushes are relieved. Estrogen also treats vaginal dryness and irritation. Women who take estrogen have fewer urinary problems, such as infection and incontinence. The symptoms of menopause may return when you stop taking HT.
Hormone therapy also has been shown to help keep bones strong, which helps prevent osteoporosis. However, it only protects bones for as long as you use it. When you stop taking HT, bone loss resumes. It is not recommended that you take HT just to prevent bone loss because the risks may outweigh the benefits. Although, if you are taking HT to relieve other symptoms of menopause, you’ll get the benefit of protecting your bones for as long as you take it. For a woman to continue to benefit, she must continue therapy. You and your doctor should decide whether this treatment is right for you.
Risks and Side Effects
As with any treatment, HT is not risk free. Estrogen therapy causes the lining of the uterus to grow and can increase the risk of uterine cancer. However, adding progestin lowers the risk of uterine cancer to less than that in women who do not take HT.
In women who take HT, spotty bleeding may occur. Some women even get heavier bleeding like that of a menstrual period. Your doctor may try adjusting your doses to minimize bleeding. Other side effects that women on HT have reported include fluid retention and breast soreness. This soreness usually lasts for a short time.
There is an increased risk of breast cancer in women who use combined hormone therapy. The increase appears to be small, but increases depending on how long a women takes hormone therapy. Hormone therapy also modestly increases the risk of heart attack, stroke, and blood clots.
A Healthy Lifestyle
Women in their 30s and 40s can make key lifestyle changes to lower their risk of health problems when they get older. Perimenopause is a good time to pay attention to your health if you haven’t been doing so all along. You will feel more in control if you take charge. This means practicing good health habits and playing an active role in your health care.
Eat a Healthy Diet
Eating a healthy diet will help you look and feel better. It also will lower your risk of osteoporosis and heart disease.
It is important to eat a well-balanced diet that contains plenty of vegetables, fruits, and grains. You also should limit your intake of fatty foods and sweets. Fat intake should be less than 30% of daily calories.
As noted earlier, a calcium-rich diet can help keep your bones strong. If you cannot get enough calcium from food, you can take calcium supplements or antacids that are high in calcium. These are sold over-the-counter in pharmacies and many grocery stores.
Exercise
Making exercise a part of your life can pay off in many ways. Exercise can help you lose weight and keep it off. Aerobic exercises help protect against heart disease and diabetes, and weight-bearing exercises help prevent osteoporosis. Regular exercise also:
- Gives you more energy
- Relieves stress
- Increases muscle strength and flexibility
- Helps you sleep better
- Improves circulation
- Lowers blood pressure
In short, exercise makes you look and feel better. If you’re not used to strenuous physical activity, it’s a good idea to check with your doctor before you start an exercise program, especially if you’re overweight or older than 40 years.
To get a good cardiovascular workout, you need to exercise at your target heart rate for 30 minutes or more most days of the week. Your target heart rate varies depending on your age. (Table 2)
Even moderate exercise will improve your health. If it’s hard to fit exercise into your busy schedule, there are things you can do to be more active. For example:
- Whenever possible, walk rather than drive.
- Take the stairs instead of the elevator.
- Get off the bus a few stops early.
- Walk during your lunch hour.
Maintain a Healthy Weight
Weight gain is not so much a result of menopause as of middle age. About 1 in 4 women aged 35–64 years is overweight. Metabolism slows as you age, so your body takes longer to burn up the food you eat. Women have about 25% body fat, compared with 15% for men. This extra fat makes it easier for women to gain weight and harder to lose it.
Target Heart Rate for Women
To find your target heart rate, look for the age category closest to your age and read the line across. For example, if you are 43, the closest age on the chart is 45; the target heart rate is 105-140 beats per minute. Your maximum heart rate is usually 220 minus your age. Your target heart rate is 60-80% of the maximum. These figures are averages to be used as general guidelines and do not apply to pregnant women.
| Age (years) | Target Heart Rate (beats per minute) | Average Maximum Heart Rate (beats per minute) |
| 20 | 120-160 | 200 |
| 25 | 117-156 | 195 |
| 30 | 114-152 | 190 |
| 35 | 111-148 | 185 |
| 40 | 108-144 | 180 |
| 45 | 105-140 | 175 |
| 50 | 102-136 | 170 |
| 55 | 99-132 | 165 |
| 60 | 96-128 | 160 |
| 65 | 93-124 | 155 |
| 70 | 90-120 | 150 |
U.S. Department of Health and Human Services; Public Health Service; National Institutes of Health; National Heart, Lung, and Blood Institute: Exercise and Your Heart. NIH Publication No. 81-1677. Washington, DC: U.S. Government Printing Office, 1981
You may gain weight when you take in more calories per day than you burn. Carrying around too much weight can decrease your energy and increase your risk of ailments. Overweight people are more likely to have heart disease, high blood pressure, diabetes, high cholesterol, and backaches.
In general, it’s best not to exceed weight guidelines for your height (Table 3). To reach your ideal weight, you should cut calories—eat a balanced diet—and get regular aerobic exercise.
Don’t try crash diets. To lose weight safely, it’s a good idea to work with your doctor and a dietitian. A healthy rate of weight loss is 1–2 pounds a week.
| Height | Weight (lbs) for Adults Older than age 35 Years |
| 5’0″ | 108-138 |
| 5’1″ | 111-143 |
| 5’2″ | 115-148 |
| 5’3″ | 119-152 |
| 5’4″ | 122-157 |
| 5’5″ | 126-162 |
| 5’6″ | 130-167 |
| 5’7″ | 134-172 |
| 5’8″ | 138-178 |
| 5’9″ | 142-183 |
| 5’10” | 146-188 |
| 5’11” | 151-194 |
| 6’0″ | 155-199 |
*Height is without shoes
*Weight is without clothes
* The higher weights generally apply to men, who tend to have more muscle and bone. The lower weights more often apply to women who have less muscle and bone.
Adapted from the U.S. Department of Agriculture, U.S. Department of Health and Human Services. Nutrition and your health: dietary guidelines for Americans. 5th ed. Washington, DC: USDA; USDHHS, 2000
Don’t Smoke
Women who smoke shorten their lives by 5–8 years. They also increase their risk of osteoporosis. Smoking doubles the risk of heart disease and cancer of the cervix and vulva in women, and multiplies the risk of lung cancer 12 times. Even the children of smokers can be affected by being exposed to secondhand smoke.
When you quit smoking, you reverse the ill effects the habit has on your body. Within a few days, your sense of smell and taste improves. Within 3 months, your circulation improves and breathing gets easier. Within 1 year, your risk of a heart attack is cut in half. Within a few years, your risk of other serious diseases related to smoking decreases to nearly that of a nonsmoker.
If you don’t think you can quit “cold turkey,” cut down slowly first. Try these approaches:
- Smoke only one half of each cigarette.
- Decide ahead of time how many cigarettes you’ll smoke during the day and only carry those with you.
- Each day, delay lighting your first cigarette by 1 hour.
- Stop buying cigarettes by the carton.
- Limit yourself to smoking a cigarette only after each meal or snack.
Once you decide to quit, avoid thinking about how hard it might be. Focus on your reasons for quitting—to improve your health, protect your family, or save money. Tell your family and friends that you plan to stop smoking and set a target date.
When that day comes, throw out all your cigarettes and get rid of your ashtrays and lighters. Clean your clothes to free them of the cigarette smell. Keep busy by going to the movies, exercising, or taking long walks. It may help to spend most of your free time in places where smoking is not allowed, such as stores, libraries, and museums.
If you feel you can’t quit on your own, ask your doctor for help. He or she can assist you or refer you to a stop-smoking program. You doctor may prescribe medication to help you quit. You also may wish to try nicotine chewing gum or patches to help wean you from your habit. Nicotine gum and patches can be bought without a doctor’s prescription in your local pharmacy.
Limit Alcohol Intake
Drinking alcohol poses special concerns for women. A woman who drinks the same amount as a man is affected more. This is because her body contains less water to dilute the alcohol and her stomach has less of the key enzyme that digests it. When you drink, the alcohol slows your reflexes and affects your judgment and memory. One important reason why perimenopausal women should watch their drinking is that alcohol interferes with bone growth and calcium absorption.
Having one to two drinks a day may be fine. Larger amounts have been linked with high blood pressure, damage to the heart muscle, and some cancers. Over time, cirrhosis—a liver disease that can cause death—may develop. Women who drink large amounts of alcohol may develop menstrual problems or start menopause earlier than normal.
Get Regular Health Care
Routine health care, even if you’re not sick, can help detect problems early. It also gives you and your doctor a chance to talk about ways to avoid problems later in life.
You should visit your doctor once a year to have regular exams and tests. Certain tests should be done regularly for all women in your age group.
During a routine exam, your doctor will measure your weight and blood pressure and may check your skin and body overall to be sure everything is normal. During a routine gynecologic exam, your doctor will check your breasts for lumps or discharge, feel your abdomen to see if there are any problems with your ovaries or uterus, inspect your vulva and vagina, and may examine your rectum.
During your exam, the doctor may ask questions about:
- Your health history
- Your diet
- Your exercise habits
- Whether you smoke or drink alcohol or use drugs
- Whether you take any medications
- Your sexual practices to see if you are at risk for sexually transmitted diseases (STDs) or pregnancy
Your regular health care also may include eye exams. Nine out of 10 women between the ages of 40 years and 64 years wear glasses or contact lenses to help them see better for reading and other close-up activities. Dental checkups are important, too. You should visit your dentist regularly to have your teeth and gums cleaned. Gum disease, a problem that can lead to tooth loss, is more common as you get older.
Do Self-Exams
Throughout the year, there are exams you can do yourself to find possible problems early. One of these is the breast self-exam. Being familiar with the usual ridges and bumps in your breasts may make it easier for you to notice any changes.
Checking your entire body for skin changes also is a good idea. Exposure to the sun or use of tanning lamps can increase the risk of skin cancer. Look for redness, swelling, or any abnormal change. Inspect any moles and pay special attention to the sizes, shapes, edges, and color. See your doctor if a mole has uneven edges, contains different shades of brown or black, or is greater in diameter than a pencil eraser.
| Routine Test | What and Why | When |
| Pap test (cervical cytology screening) | A sample of cells taken from the cervix during a pelvic exam to look for changes that could lead to cancer | Annually, or every 2-3 years after 3 normal tests in a row, if low risk |
| Lipid profile assessment | A blood test that checks levels of cholesterol (a substance that helps carry fat through the blood vessels) because levels that are too high can lead to hardening of the arteries | Every 5 years beginning at age 45 years |
| Mammography | An X-ray of the breast to look for breast cancer | Every 1-2 years beginning at age 40 years; yearly beginning at age 50 years |
| Colorectal cancer screening | Screening may be done with fecal occult blood test (FOBT), flexible sigmoidoscopy, colonoscopy, or double contrast barium enema to look for cancer | Yearly FOBT or sigmoidoscopy every 5 years or yearly FOBT plus sigmoidoscopy every 5 years or double contrast barium enema every 5 years or colonoscopy every 10 years beginning at age 50 years |
| Fasting glucose testing | A test to measure the level of glucose (a sugar that is present in the blood and is the body’s main source of fuel) because if it is too high it could signal diabetes | Every 3 years after age 45 years |
| Thyroid-stimulating hormone screening | A blood test that checks to make sure the thyroid gland is functioning properly | Every 5 years beginning at age 50 years |
| Flu vaccine | A shot to help prevent the flu (influenza) | Once a year beginning at age 50 |
| Tetanus-diphtheria booster | A shot to help prevent tetanus and diphtheria | Once every 10 years |
Use Birth Control
Although your menstrual periods may become erratic as you get closer to menopause, pregnancy is still possible. Even having other signs of perimenopause, such as hot flushes, does not mean you can’t get pregnant. About 75% of pregnancies in women older than 40 years are unplanned. You are not completely free of the risk of pregnancy until 1 year after your last period.
It’s important to use a form of birth control that fits your needs. Many options are open to you:
- Hormonal methods—include pills, the patch, the vaginal ring, injections (safe for women older than 40 years who are healthy and don’t smoke)
- Intrauterine device (IUD)
- Barrier methods—include the diaphragm, male and female condom, and spermicides
- Sterilization—blocking, sealing, or cutting the fallopian tubes for women and vasectomy for men
Not having sex at certain times in the menstrual cycle is a natural family planning method used by some women. You should not rely on this method during perimenopause if your menstrual cycle is the least bit irregular.
Get Preconceptional Counseling
If you are planning a pregnancy late in your childbearing years, be aware that the risk of problems increases with the woman’s age. A woman younger than age 50 years should take 0.4 mg of folic acid daily if she is planning a pregnancy. It’s also important toreceive preconceptional counseling.
Having a first child near or after age 40 years is not rare. Women who get pregnant in their 40s can have safe pregnancies and healthy babies. However, it may be more difficult to become pregnant and risks are increased for both the woman and the baby.
Practice Safer Sex
Everyone who is sexually active is at risk of getting an STD. Some STDs, such as syphilis or chlamydia, usually can be cured. Others have no known cure. Among these is acquired immunodeficiency syndrome (AIDS), a life-threatening disease caused by human immunodeficiency virus (HIV).
The best protection from STDs is for a couple to have sex only with each other. If either of you does have sex with others, make sure to use a latex condom every time. Limit your number of partners and ask about their sexual history. Avoid sex if you or your partner suspect either of you has an STD.
Finally…
There was a time when no one talked about menopause; it was a mystery to most women. Today, you can find a wealth of information on the topic. Talk with your doctor and learn as much as you can. That way, you can look ahead to the next stage of life with confidence. If you feel good about yourself, make wise choices, and lead a healthy lifestyle, you’ll be better able to cope with this midlife transition.
Glossary
Acquired Immunodeficiency Syndrome (AIDS): A group of signs and symptoms, usually of severe infections, occurring in a person whose immune system has been damaged by infection with human immunodeficiency virus (HIV).
Corticosteroids: Hormones given to mature fetal lungs, for arthritis, or other medical conditions.
Estrogen: A female hormone produced in the ovaries that stimulates the growth of the lining of the uterus.
Fecal Occult Blood Test (FOBT): A test of a stool sample for blood, which could be a sign of cancer of the colon or rectum.
Human Immunodeficiency Virus (HIV): A virus that attacks certain cells of the body’s immune system and causes acquired immunodeficiency syndrome (AIDS).
Impotence: The inability in a male to achieve an erection or to sustain it until ejaculation or until intercourse takes place.
Menopause: The stage in a woman’s life when ovaries stop functioning and menstruation stops.
Osteoporosis: A condition in which the bones become so fragile that they break more easily.
Ovaries: Two glands, located on either side of the uterus, that contain the eggs released at ovulation and produce hormones.
Perimenopause: A transitional phase before menopause that usually extends from age 45 years to 55 years.
Progesterone: A female hormone that is produced in the ovaries and matures the lining of the uterus. When its level decreases, menstruation occurs.
Progestin: A synthetic form of progesterone that is similar to the hormone produced naturally by the body.
Sigmoidoscopy: A test in which a slender device is placed into the rectum and lower colon to look for cancer.
Vasectomy: A method of male sterilization in which a portion of the vas deferens is removed.
