Bowel control problems affect at least 1 million people in the United States. Loss of normal control of the bowels is called fecal incontinence. This leads to leakage of solid or liquid stool (feces) or gas.
Many women are not comfortable talking about bowel control problems. They may think that nothing can help them. If you talk with your doctor about it, he or she can offer effective treatments. This page will explain:
- The causes of bowel control problems
- How they are diagnosed
- How you can help regain control of your bowels
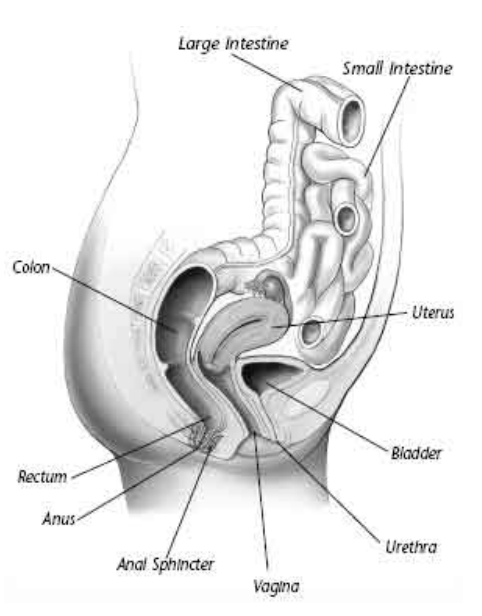
Bowel Control
Normal bowel function requires healthy muscles and nerves in the rectum and pelvis. Problems in this area can lead to fecal incontinence (loss of bowel control). Common problems include:
- Injury to the anal sphincter muscles—this can cause stool or gas to leak from the rectum.
- Loss of feeling in the rectum—this can make it hard to tell when it is time to have a bowel movement.
- Inability of the rectum to stretch and store stool—this may make it hard to hold a bowel movement until you can get to the bathroom.
Bowel control problems occur up to eight times more often in women than in men. The problem also is more common in older people or in women who have just given birth. It can occur at any time in a person’s life.
Many women are not comfortable talking about incontinence with their doctors. For this reason, the problem often goes without treatment.
Causes
The most common cause of bowel control problems is childbirth. This is because as the baby passes through the vagina, the muscles or the nerves near the rectum may be stretched or torn.
Some women have short-term loss of bowel control right after childbirth. It likely will improve within a few days. In other cases, it does not occur until many years later. As a person ages, the anal sphincters may weaken. A minor problem in a younger woman can become worse in later life. Bowel control problems can be linked to:
- Stools that are too loose (diarrhea)
- Stools that are too hard (constipation)
- Certain medications
- Certain illnesses such as diabetes, multiple sclerosis, or stroke (they can damage the nerves to the rectum and cause loss of feeling)
- Problems with the gastrointestinal system, such as inflammatory bowel disease, irritable bowel syndrome, colitis, or cancer of the rectum
- Surgery or radiation therapy to the pelvic area
- Certain sexual practices, such as anal intercourse
Symptoms
A woman with a bowel control problem may have gas or leak liquid or solid stool. Other symptoms may include:
- A strong or urgent need to have a bowel movement
- Stool spotting on underwear or pads
- Diarrhea
- Constipation
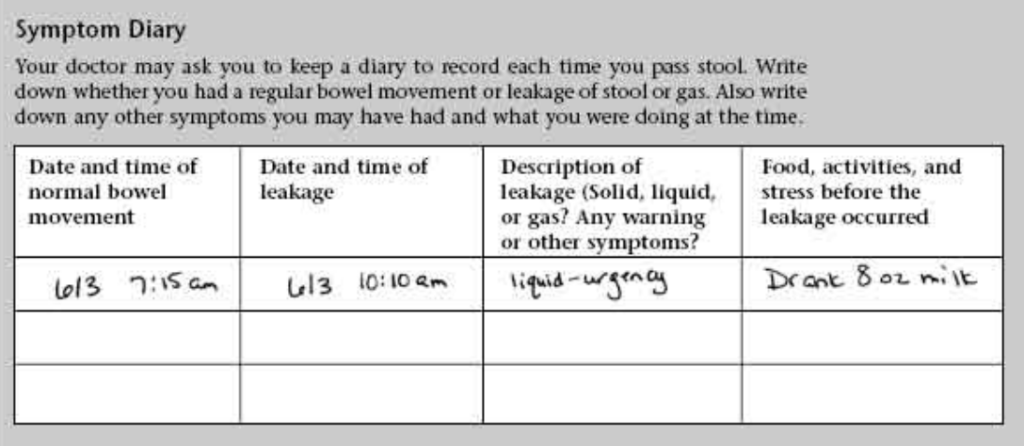
Problems may occur often or only once in a while. Your doctor may ask you to keep a symptom diary to describe your bowel movements and record when they occur. Be sure to write in your diary when you leak gas or stool (see box). In some women, fecal incontinence occurs with urinary incontinence (not being able to control urine). Some treatments for bowel problems also will help urine problems.
Diagnosis
To try to find the cause of your problem, your doctor will ask you questions about your medical history. Describe your symptoms clearly. Be open and honest. Tell your doctor about any prescription or over-the-counter products or herbal remedies you may be taking. This will help your doctor find the best treatment for you.
The doctor will examine your vagina, anus, and rectum. He or she will look for signs of problems, such as loss of normal nerve reflexes or muscle tone.
Tests may be needed to help find the cause:
- Use of a scope to see inside the rectum
- Anorectal manometry to test the strength of the anal muscles. A small sensing device is placed into the anus. The device records changes in pressure as you relax and tighten the anal muscles.
- Proctography tests to find out how much stool the rectum can hold and how well it holds and gets rid of the stool.
- A test to check if the nerves to the rectum and anus are working as they should
- Ultrasound pictures from inside the rectum to check the anal muscles Your doctor may work with other doctors to manage your care.
Treatment
Once the cause of the problem is known, you and your doctor can discuss the best treatment for you. The type of treatment depends on the cause and how severe the problem is.
Your doctor may suggest certain lifestyle changes to help you control your bowels. For instance, the problem may be treated by changes in your diet and simple home exercises to strengthen the anal muscles.
If a disease is causing the problem, proper treatment may improve symptoms. In some cases, surgery is needed to correct the problem.
Regular Bowel Habits
Having regular bowel movements helps to prevent diarrhea or constipation. If you have diarrhea, your doctor will help you find out if certain foods, such as dairy products, trigger loose stools. Not eating these foods may help prevent loss of control.
If you have constipation, your doctor may suggest more exercise. He or she also may suggest some changes in your diet, such as eating more fruits and vegetables and drinking plenty of water. Slowly increase your fiber intake to 35–40 grams a day.
If a certain medication is causing diarrhea or constipation, your doctor may change your dosage or switch to another medication. In some cases, he or she may prescribe a medication to prevent diarrhea or constipation and help you have regular bowel movements.
Muscle Exercises
Your doctor may suggest you do Kegel exercises. Kegel exercises strengthen the muscles that surround the openings of the rectum, urethra, and vagina. Your doctor can help ensure you are doing the exercises the correct way (see box).
Biofeedback Training
With biofeedback, you learn to contract the anal muscles with the help of a recording device. The device measures the strength of your contractions. A monitor shows you how well you are doing. Biofeedback can help you learn to tighten your anal muscles when you sense stool or gas in the rectum.
Surgery
In some cases, surgery may help correct loss of bowel control. If the sphincter muscle of the rectum is damaged, it often can be treated with surgery. If the colon, rectum, or anus cannot function, in rare cases a colostomy may be needed so the body can get rid of the waste. Your doctor will help you decide if surgery may be an option for you.
Skin Care
Leakage of stool can irritate the skin around the anus. Find a type of cleanser that does not irritate your skin. Make sure to keep the area dry. Dampness can lead to irritation or a yeast infection. There are special creams, liquids, and powders for people with incontinence that can help protect skin. Tell your doctor if you develop a skin rash, irritation, or itching.
Kegel Exercises
Kegel exercises are used to strengthen the muscles that surround the openings of the rectum, vagina, and urethra. Just like doing sit-ups to flatten your abdomen, these exercises only work when the right muscles are used, the “squeeze” is held long enough, and enough repetitions are done.
Your doctor or nurse will ask you to squeeze your sphincter muscles as if you were stopping a bowel movement. When you begin the exercise program, place a hand on your abdomen to make sure you do not squeeze those muscles. Also do not squeeze your thighs or buttocks.
Squeeze your pelvic muscles for 10 seconds, 10–20 times in a row. Your doctor will tell you how many times a day to perform the exercises and how long you should keep doing them.
Finally…
Many women are not comfortable talking about incontinence with their doctors. For this reason, the problem often goes without treatment. If you know or suspect you have a bowel control problem, tell your doctor about your symptoms. Much can be done to help you regain control of your bowels.
Glossary
Bowels: The small and large intestines, which are digestive organs.
Colitis: A disease that causes inflammation of the colon, the last part of the large intestine.
Colostomy: An opening that connects the colon to the surface of the abdomen, which provides a new way for waste and gas to leave the body.
Diabetes: A condition in which the levels of sugar in the blood are too high.
Inflammatory Bowel Disease: A term for several diseases that cause inflammation of the intestines.
Irritable Bowel Syndrome: A noninflammatory condition of the bowels that may cause cramping, diarrhea, or constipation.
Kegel Exercises: Pelvic muscle exercises that assist in bladder and bowel control.
Multiple Sclerosis: A disease of the nervous system that leads to loss of muscle control.
Sphincter Muscle: A muscle that can close a bodily opening, such as the sphincter muscle of the rectum.
Stroke: A sudden interruption of blood flow to all or part of the brain, caused by blockage or bursting of a blood vessel in the brain and often resulting in loss of consciousness and temporary or permanent paralysis.
Ultrasound: A test in which sound waves are used to examine internal structures. During pregnancy, it can be used to examine the fetus.
Urethra: A short, narrow tube that conveys urine from the bladder out of the body.
Vagina: A passageway surrounded by muscles leading from the uterus to the outside of the body, also known as the birth canal.
