Many women feel physical or mood changes during the days before menstruation. When these changes affect a woman’s normal life, they are known as premenstrual syndrome(PMS).
Premenstrual syndrome can affect menstruating women of all ages and backgrounds. The cause of PMS is unclear. However, the symptoms can be managed in many women.
This page explains:
- how PMS can affect you
- conditions that mimic PMS
- treatments, including self-treatments and medications
How PMS Can Affect You
Premenstrual symptoms are a common part of the menstrual cycle. In fact, at least 85% of women who menstruate have at least one premenstrual symptom.
Women with PMS experience a pattern of symptoms month after month. Sometimes, these symptoms interfere with their daily lives.
To diagnose PMS, a health care provider must confirm a pattern of symptoms. A woman’s symptoms must:
- be present in the 5 days before her period for at least three menstrual cycles in a row
- end within 4 days after her period starts
- interfere with some of her normal activities
Some common symptoms of PMS are emotional. Some are physical. Keeping a record of your symptoms can help your health care provider decide if you have PMS (see “Keeping a Symptom Record”). Each day for at least 2–3 months, write down and rate any symptoms you feel. Record the dates of your periods as well.
This simple record can help your health care provider learn if you have a pattern of symptoms. It will help your health care provider diagnose PMS or perhaps some other condition.
Keeping a Symptom Record
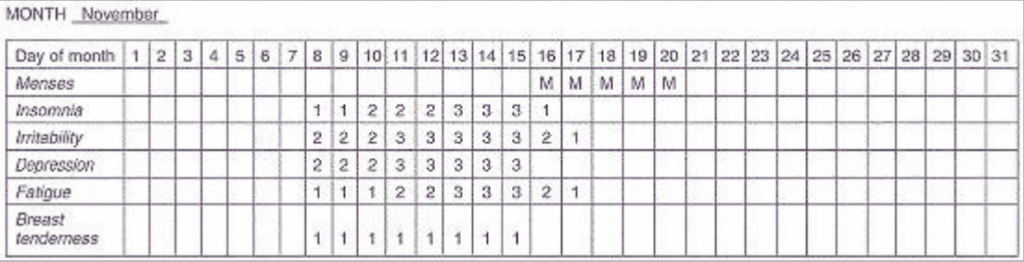
A symptom record can help your health care provider decide what treatment is best for you. Keeping a record is easy. Write your symptoms on a calendar, or use a chart like the one shown below. Keep a record for 2–3 months.
Instructions:
- Record up to five symptoms that are bothersome.
- At the end of each day, rate each symptom as mild (1), moderate (2), or severe (3).
- If you have no symptoms, leave the space for that day blank.
- For the row labeled “menses,” put an “M” in the box of each day you have menstrual bleeding.
The following are common PMS symptoms that you can use in your record:
Emotional symptoms:
- Depression
- Angry outbursts
- Irritability
- Crying spells
- Anxiety
- Confusion
- Social withdrawal
- Poor concentration
- Insomnia
- Increased nap taking
- Changes in sexual desire
Physical symptoms:
- Thirst and appetite changes (food cravings)
- Breast tenderness
- Bloating and weight gain
- Headache
- Swelling of the hands or feet
- Aches and pains
- Fatigue
- Skin problems
- Gastrointestinal symptoms
- Abdominal pain
Example of a completed record:
Conditions That Mimic PMS
Symptoms of other conditions can mimic PMS or overlap with PMS. Some of these conditions are
- depression
- anxiety
- perimenopause
- chronic fatigue syndrome
- irritable bowel syndrome
- thyroid disease
Depressive and anxiety disorders are the most common conditions that overlap with PMS. About one half of women seeking treatment for PMS have one of these disorders. The symptoms of depression and anxiety are much like the emotional symptoms of PMS. Women with depression, however, often have symptoms that are present all month long. These symptoms may worsen before or during their periods. Your health care provider will want to find out whether you have one of these conditions if you are having PMS symptoms.
In addition to depression and anxiety, symptoms of other disorders can get worse right before your period. Some of the most common conditions that may worsen before menstruation are:
- seizure disorders
- migraines
- asthma
- allergies
If your symptoms are severe and are causing problems with work or personal relationships, you may have premenstrual dysphoric disorder (PMDD) (see “Premenstrual Dysphoric Disorder”). PMDD is a severe type of PMS that affects a small percentage of women. Treatment is available that can help relieve the symptoms of PMDD.
Premenstrual Dysphoric Disorder
A woman has PMDD when she has five or more of the following symptoms:
- Feeling depressed
- Feeling tense, anxious, or “on edge”
- Moodiness or frequent crying
- Constant irritability and anger that cause conflict with other people
- Lack of interest in things you used to enjoy
- Having problems concentrating
- Lack of energy
- Appetite changes, overeating, or cravings
- Having trouble sleeping or sleeping too much
- Feeling overwhelmed
- Physical symptoms such as tender or swollen breasts, headaches, joint or muscle pain, bloating, and weight gain
Most of the time, symptoms begin the week before a woman’s period and end a few days after her period starts. A symptom record will help your health care provider decide if you have PMDD.
Drugs called selective serotonin reuptake inhibitors (SSRIs) can help treat PMDD in some women. These
drugs are used to treat depression.
Treatment
If your symptoms are mild to moderate, they often can be relieved by changes in lifestyle or diet. If your PMS symptoms begin to interfere with your life, you may decide to seek medical treatment. Treatment will depend on how severe your symptoms are. In more severe cases, your health care provider may recommend medication.
Talk with your health care provider about your symptoms and treatment options. He or she may suggest some of the options described here. You may have to combine options to find relief.
Lifestyle Changes
If you have mild to moderate symptoms, there are steps you can take on your own to relieve them. These changes in lifestyle also can help women with more severe PMS.
Aerobic Exercise. For many women, regular aerobic exercise lessens PMS symptoms. It may reduce fatigue and depression. Aerobic exercise, which includes brisk walking, running, cycling, and swimming, increases your heart rate and lung function. Exercise regularly, not just during the days that you have symptoms. A good goal is at least 30 minutes of exercise most days of the week.
Relaxation. Finding ways to relax and reduce stress can help women who have PMS. Your health care provider might suggest relaxation therapy to help lessen PMS symptoms. Relaxation therapy may include breathing exercises, meditation, and yoga. Massage therapy is another form of relaxation therapy that you may want to try. Some women find therapies like biofeedback and self-hypnosis to be helpful.
Getting enough sleep is important. Regular sleeping habits—in which you wake up and go to sleep at the same times every day, including weekends—may help lessen moodiness and fatigue.
Dietary Changes. Simple changes in your diet may help relieve the symptoms of PMS. A diet rich in complex carbohydrates may reduce mood symptoms and food cravings. Complex carbohydrates are found in foods made with whole grains, like whole wheat bread, pasta, and cereals. Other examples are barley, brown rice, beans, and lentils. Add calcium-rich foods, like yogurt and leafy green vegetables, to your diet. Reduce your intake of fat, salt, and sugar. Avoid caffeine and alcohol.
Some health care providers suggest that you eat six small meals a day rather than three large ones. Another way is to eat slightly less at your three meals and add three light snacks. Keeping your blood sugar level stable will help with symptoms. When adding foods to your diet to treat symptoms, though, be sure to reduce calories in other areas to avoid weight gain.
Support. Simply having information about PMS and its symptoms can help you understand what is happening and reduce your anxiety about how you are feeling. Being aware of your symptoms may help prevent conflicts with others. Even talking with others about what you are going through can help. Sharing your feelings may help your family to support you more.
Dietary Supplements
Dietary supplements may help lessen the symptoms of PMS in many women. Your health care provider may suggest that you take calcium supplements. Studies have shown that taking 1,200 mg of calcium a day can help reduce the physical and mood symptoms that are part of PMS.
Although the evidence is limited, taking magnesium supplements may help reduce water retention (“bloating”), breast tenderness, and mood symptoms. One study has shown that vitamin E also may help reduce symptoms of PMS.
There are many products that are advertised to help with PMS. Most of these products have either not been tested or have not been proved to be effective. It is important to talk with your health care provider before taking any PMS product or supplement. Taking excess amounts of them or taking them with some medications may be harmful.
Medications
Women with severe PMS may not feel relief with lifestyle or dietary changes alone. If these changes do not reduce symptoms, your health care provider may suggest medications.
Drugs that prevent ovulation, such as hormonal contraceptives, may lessen physical symptoms. However, not all may relieve the mood symptoms of PMS. It may be necessary to try more than one of these medications before finding one that works.
Antidepressants can be helpful in treating PMS. These drugs can help lessen mood symptoms. They can be used 2 weeks before the onset of symptoms or throughout the menstrual cycle. There are many kinds of antidepressants. If one does not work for you, your health care provider may prescribe another. However, for some women, antidepressants are not helpful in treating PMS symptoms.
If anxiety is a major PMS symptom for you, an antianxiety drug can be tried if other treatments do not seem to help. These drugs are taken as needed when you have symptoms.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help reduce pain. Talk with your health care provider before taking NSAIDs. Long-term use of NSAIDs may cause stomach bleeding or ulcers.
Diuretics (“water pills”) are drugs that help reduce fluid buildup. Your health care provider can prescribe a diuretic if water retention is a major symptom for you. Tell your health care provider what other drugs you are taking, especially NSAIDs. Using NSAID and diuretics at the same time may cause kidney problems.
Finally…
Finding the right PMS treatment may take some time and involve trying different options. Many women with PMS find relief with exercise, diet, and other lifestyle changes. If these measures do not bring relief, see your health care provider. Several medications are available that are helpful in managing PMS. It also is important to find out whether you have other conditions that are easily confused with or overlap with PMS.
Glossary
Antidepressants: Medications used to treat depression.
Depression: Feeling of sadness for periods of at least 2 weeks.
Diuretics: Drugs given to increase the production of urine.
Menstruation: The monthly discharge of blood and tissue from the uterus that occurs in the absence of pregnancy.
Ovulation: The release of an egg from one of the ovaries.
Perimenopause: The period around menopause that usually extends from age 45 years to 55 years.
Source: acog.org
