Certain health problems can affect the vulva (the outer part of the female genital area). Some problems are minor. Others are more serious. Finding and treating changes early can help prevent more serious problems. You can help find problems by doing a vulvar self-exam. This page will explain:
- How to examine your vulva
- Signs of a problem
- Types of vulvar problems and how they are treated
The earlier you seek treatment, the better your chances of treating the problem with success.
The Vulva
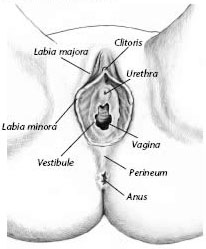
The outside of the female genital area is called the vulva. The fleshy part of this area that lies directly over the pubic bone is called the mons veneris. The outer lips of the vulva are called the labia majora. The inner lips are called the labia minora. The clitoris is at the top of the inner lips. For most women, the clitoris is a center of sexual pleasure. It is partly covered by a fold of tissue called the hood. The perineum is the area between the anus and vagina. The vestibule is found within the inner lips. The vagina and the urethra open into the vestibule. Just inside the vestibule are the openings to the glands that make lubrication.
How to Find Vulvar Problems
Just as you would examine your breasts or skin for changes, you should examine your vulva. A good way to screen for vulvar problems is to do a vulvar self-exam once a month.
Why Should I Do a Self-Exam?
2. Gently separate the outer lips of the vulva. Look for any changes or signs of a problem.
3. Next, separate the inner lips and look at the area between them. Also look at the entrance to the vagina.
4. Gently pull back the hood of the clitoris and examine the area under the hood and the tip of the clitoris.
5. Be sure to inspect the area around the urethra, the perineum, the anus, and the outside of the labia majora.
The vulvar self-exam will help you to be aware of any changes that could signal a problem. This exam is even more vital if you have ever had a vulvar problem. Some changes in the vulva may be an early sign of cancer.
What Am I Looking For?
When you examine your vulva, you should look for:
- Redness
- Swelling
- Dark or light spots
- Blisters
- Bumps
- Any other changes
Tell your doctor if you see any changes or have symptoms that do not go away. Symptoms include:
- Itching
- Bleeding
- Discomfort
- Burning
If a problem does occur, you are more likely to find it at an early stage if you check yourself on a regular basis.
Care of the Vulva
To help clear up certain vulvar problems or prevent them from coming back, your doctor may ask you to do the following:
- Keep the vulva clean and dry
- Do not wear tight-fitting pants or underwear. Wear only cotton underwear.
- Do not wear pantyhose (unless they have a cotton crotch).
- Do not use pads or tampons that have deodorant or a plastic coating.
- Do not use perfumed soap or scented toilet paper.
- Do not douche or use feminine sprays or talcs.
- Do not sleep in tight-fitting garments.
Types of Vulvar Problems
If you have any symptoms or detect signs of a problem, see your doctor. To find the cause, your doctor will ask you some questions. He or she also will examine you, and tests may be needed.
There are a number of problems that may occur on the vulva. Many problems of the vulva share the same symptoms.
Yeast Infections
Yeast infections are the most common type of vulvar infections. The vagina often is infected, too. Symptoms of yeast infection include redness, itching, and a whitish, clumpy discharge. A burning feeling also may occur when you urinate.
To diagnose a yeast infection, a sample of the discharge may be taken and studied under a microscope. Good hygiene and antifungal drugs are the recommended treatment. A cream or tablet (or both) can be inserted into the vagina or applied to the vulvar skin. These drugs can be bought over-the-counter. Some doctors may prescribe a single dose that you take by mouth. If the symptoms do not go away after treatment, call your doctor.
Contact Dermatitis
Contact dermatitis is caused by irritation of the skin of the vulva. Some items that may cause contact dermatitis are listed . It is not always easy to find the cause.
The main symptoms of contact dermatitis are redness and itching. To diagnose it, your doctor will examine the vulvar area and ask you about the things that come in contact with your vulva. Getting rid of the source of the irritation is the first step in treating this problem.
Causes of Contact Dermatitis
Contact Dermatitis is caused by irritation of the skin of the vulva. It may be caused by:
- Perfumed or dyed toilet tissue
- Underwear or bathing suits
- Soaps, detergents, or fabric softeners
- Talcum powder
- Feminine hygiene sprays
- Deodorant pads
- Spermicidal foams, creams, or jellies
- Rubber products, such as diaphragms or condoms
- Poison ivy or similar plants or talcs
- Sleeping in tight-fittings garments
Sexually Transmitted Diseases
Sexually transmitted diseases (STDs) can affect the vulva. If you are sexually active, the best way to reduce the chance of getting or spreading an STD is to use a latex condom. The most common STDs that affect the vulva are genital warts and genital herpes.
Genital Warts. Genital warts (condyloma), like warts on other parts of the body, are caused by the human papillomavirus (HPV). They are spread through sexual contact. The warts appear on the vulva as raised and sometimes reddened patches that may hurt or itch. Sometimes there may be a cluster of warts that look like tiny cauliflowers. Warts can be treated with medication applied to the area or surgery to remove them. The type of treatment depends on where the warts are located.
Genital Herpes. Genital herpes infection is caused by the herpes simplex virus. It usually is spread through sexual contact. Often there are mild symptoms or none at all. In other cases, symptoms are severe. The infection is marked by sores, blisters, or ulcers that appear on the vulva. They can last from a few days to a few weeks, then may go away and come back. They can cause pain, discomfort, and itching. There may be no symptoms at the time of infection. Later outbreaks often are less severe than the first outbreak.
There is no cure for genital herpes. However, there are medications that can help control outbreaks, relieve symptoms, and prevent spreading the virus.
Problems in Other Areas
Problems that affect other parts of the body also may affect the vulva. Psoriasis, for instance, is a skin disease that can appear on the vulva as red, thick, scaly patches that may itch. A first sign of Crohn’s disease, in which ulcers form in the digestive system, may appear as sores on the vulva. Women with diabetes often have yeast infections.
If the main disease is treated, vulvar symptoms often go away as well. If not, the vulvar symptoms are treated with creams or ointments.
Vulvodynia
Vulvodynia means “vulvar pain.” The symptoms of vulvodynia include burning, stinging, irritation, or rawness. To find the cause, your doctor will ask you questions about your pain, examine the vulva to identify painful areas, and may take a sample of fluid from the vagina. The sample then is studied under a microscope to find out whether you have an infection. Infections often can be treated with medication.
There are many methods of treatment to relieve symptoms. No one method works all the time for all women. Vulvodynia may require long-term treatment.
Vulvar Dystrophy
Vulvar dystrophy is the growth of abnormal skin on the vulva. The skin can be too thin (lichen sclerosus), too thick (hyperplasia), or a mixture of both. When it is too thin, the skin may look like thin, wrinkled paper, and the vaginal opening may shrink. When it is too thick, hardened patches may appear on the vulva. Symptoms include redness or whiteness, itching, and burning.
A biopsy may be done to diagnose this problem. Vulvar dystrophy requires long-term treatment with creams or ointments that are rubbed into the vulvar tissue.
Cancer
Most cancers of the vulva are a type of skin cancer. In their earliest form, they are precancer. Precancer means it may turn into cancer if it is not found and treated early. If skin cells are found in this stage, they are called VIN (vulvar intraepithelial neoplasia). In later stages, cancer can become invasive (spread and invade other parts of the body). Rarely, other types of cancer develop on the vulva:
- Melanoma, an advanced form of skin cancer, can occur on the vulva. In most cases, it starts with a small, mole-like growth. The growth gets bigger, changes color, or gets darker. It may grow in an irregular – not round – shape and bleed easily. Any bumps, patches, or growths on the vulva may need to be removed.
- Adenocarcinoma can arise with a condition called Paget’s disease. This cancer may look like eczema (patches of red, scaly, itchy skin) on the vulva.
Vulvar cancers most often occur in white women older than 60 years. This type of cancer occurs most often in areas of the vulva where there is chronic inflammation or VIN. Symptoms include:
- Itching of the vulva
- Burning, pain, or other discomfort in the area
- Changes in skin color (parts of the vulva can look white, red, or brown to black)
Sometimes a tumor or ulcer is present. The lymph nodes in the groin also may be enlarged. Invasive cancer of the vulva is diagnosed by biopsy. Surgery often is needed to remove all cancerous tissue. In choosing the best type of surgery, you and your doctor will discuss the impact on sexual function and the need to remove all the cancer. Types of surgery include:
- Wide local excision (cutting away the cancer and an area of normal-appearing skin around it)
- Vulvectomy (removal of the vulva including the vaginal lips, also called labia, and clitoris)
The type of treatment you receive depends on the stage of cancer. Radiation therapy also may be used to treat cancer. Chemotherapy may be used to treat more severe cancers.
Finally…
The vulvar self-exam can help alert you to vulvar problems. Talk to your doctor about any changes or symptoms you notice. The earlier you seek treatment, the better your chances of treating the problem with success.
If you are experiencing signs or symptoms of this issue, or have questions, you can schedule an appointment with us at our Baldwin Park office in Orlando, FL.
Glossary
Chemotherapy: The treatment of cancer using certain drugs to destroy malignant cells.
Inflammation: Pain, swelling, redness, and irritation of tissues in the body
Lymph Nodes: Small glands that filter the flow of lymph (a nearly colorless fluid that bathes body cells) through the body.
Radiation therapy: Treatment by exposing the affected area to high-energy radiation.
Sexually Transmitted Diseases (STDs): Diseases that are spread by sexual contact, including chlamydial infection, gonorrhea, genital warts, herpes, syphilis, and infection with human immunodeficiency virus (HIV, the cause of acquired immunodeficiency syndrome [AIDS]).
Source: acog.org
